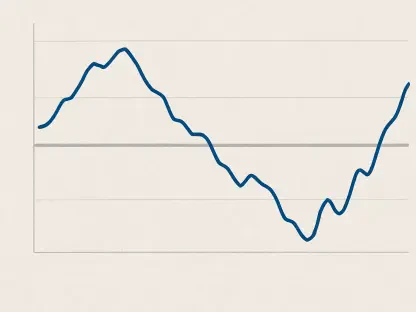
The rising cost of electricity poses significant challenges for individuals relying on in-home durable medical equipment (DME). Devices such as oxygen concentrators, CPAP machines, ventilators, and peritoneal dialysis machines are vital for maintaining health, yet their operation can substantially increase household energy bills. Monthly expenses may jump by up to 40%, particularly in states like Hawaii, California, and Massachusetts, where electricity rates are already high. This financial burden can restrict access to necessary medical devices, threatening the health and well-being of those who need them most.
Financial Strain and Health Implications
Impact on Vulnerable Populations
Research highlights that patients dependent on DMEs often find themselves energy insecure due to compromised health and strained financial conditions. This double impact not only stresses household budgets but also can deter individuals from using essential medical devices. The financial burden can range anywhere from $120 to over $700 annually, depending on device type, usage frequency, and local electricity prices. This burden makes it increasingly difficult for low-income families to manage their health needs, as energy insecurity might lead them to reduce usage or seek dangerous alternatives. Vulnerable populations face the most pressure, and there is growing concern about the adverse health outcomes linked to rationing access to medical devices.
Cost of Living vs. Quality of Life
While at-home treatments offer enhanced quality of life, the financial strain they impose should not be overlooked. For many patients, the mere presence of a necessary device at home does not guarantee its use. The gap between health-related expenses covered by Medicare and Medicaid and unaddressed electricity costs further exacerbates the problem. Patients may choose to underutilize or stop using their equipment altogether, which can directly affect their health outcomes. Insurance providers have yet to acknowledge these indirect costs, leaving households to shoulder the expenses alone. The need for expanded health insurance coverage to include energy costs is an urgent call for policymakers.
Intersection of Healthcare and Energy Needs
Call for Policy Changes
Research conducted by Indiana University, Regenstrief Institute, University of Pennsylvania, and Yale University argues that policymakers should consider expanding health insurance coverage to address the hidden costs associated with DMEs. Tightening protections against electricity disconnection is crucial, especially for households using medical equipment that relies on a continuous power supply. Moreover, reviewing and adapting insurance policies to encompass these electricity costs could alleviate significant stress. By addressing these gaps, the connection between healthcare and energy needs can be managed more effectively. This proactive approach would relieve some of the economic pressures that disproportionately affect low-income homes.
Broader Implications of Energy Insecurity
Energy insecurity extends beyond the inability to power medical devices, often forcing households into risky choices such as using a kitchen oven for heating. Such coping strategies, born out of necessity, highlight the serious implications of not addressing energy costs in healthcare discussions. The intersections between healthcare needs and basic utilities demand broader consideration, as neglecting these facets can lead to compounded health issues and safety hazards. Policymakers, therefore, must delve deeper into real-world settings and user experiences to better understand how energy insecurity affects those reliant on DMEs daily. Investigating these experiences offers a pathway to comprehensive solutions within both energy policy and healthcare frameworks.
Reassessing Healthcare Costs
Including Energy Expenses in Healthcare
The comprehensive investigation calls for redefining healthcare costs to include both direct medical expenses and associated energy costs tied to them. Addressing energy expenditures as legitimate healthcare expenses could significantly enhance the lives of individuals using DMEs. Re-evaluating insurance coverage to incorporate these costs would provide tangible relief and ensure that the critical benefits of at-home medical devices are fully realized. This shift acknowledges the hidden financial struggles that individuals face and offers a path toward securing basic healthcare necessities within sustainable financial means.
Future Considerations and Solutions
The escalating costs of electricity present significant challenges for individuals dependent on in-home durable medical equipment (DME). Essential devices like oxygen concentrators, CPAP machines, ventilators, and peritoneal dialysis machines are crucial for these individuals’ health management. However, their continuous operation can lead to a substantial rise in household energy bills, with monthly expenses potentially increasing by up to 40%. This increase is especially prominent in states such as Hawaii, California, and Massachusetts, where electricity rates are already among the highest in the nation. This financial strain could limit access to essential medical devices, thereby compromising the health and well-being of the most vulnerable individuals who rely on them. As electricity prices continue to rise, there is growing concern about the sustainability of home-based healthcare for those who need these devices to survive, emphasizing the urgent need for policy interventions to aid these households.