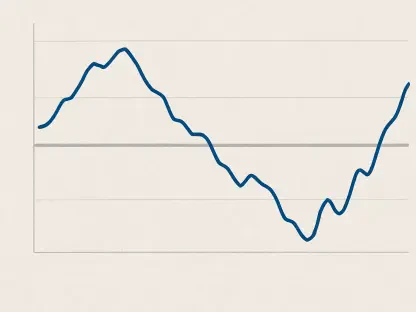
Predictive healthcare analytics has emerged as a transformative force in the healthcare industry, driving smarter and more informed decision-making processes. This field leverages advanced techniques such as artificial intelligence (AI), machine learning (ML), data mining, and statistical modeling to forecast future health outcomes based on historical data. With an emphasis on predictive capabilities rather than retrospective analysis, this burgeoning field anticipates trends and identifies potential risks, thereby allowing for timely and targeted interventions. The global market for predictive analytics in healthcare was valued at $11.7 billion in 2022 and is expected to maintain a growth trajectory with a CAGR of 24.4% through 2030, reflecting its expanding adoption across the industry.
The Evolution of Patient Care Through Data
Harnessing Multiple Data Sources
Analyzing patient care has evolved significantly with the vast amount of data available today. Predictive healthcare analytics taps into multiple data sources such as Electronic Health Records (EHRs), insurance claims, medical imaging, and health surveys. Through these data streams, predictive tools can, for example, analyze patterns in patient records to determine the likelihood of hospital readmissions or assess medication adherence to predict the onset of chronic diseases. This approach translates into more effective and timely interventions by healthcare providers. Additionally, predictive analytics allows healthcare professionals to navigate patient records more efficiently, facilitating targeted interventions and streamlining healthcare processes.
Combining different data sources can provide a comprehensive view of a patient’s health trajectory. For instance, integrated data from EHRs and medical imaging can reveal patterns that single data sources might miss. Predicting the onset of diseases like heart conditions or diabetes can thus be achieved by analyzing diverse datasets in unison, which can offer a holistic perspective. This enables healthcare providers to make well-informed decisions, optimizing patient care and minimizing risks associated with delayed diagnosis and treatment.
The Predictive Analytics Process
The process of predictive analytics in healthcare comprises three main steps: data collection, data analysis, and prediction. Initially, information is gathered from diverse sources, including EHRs, patient registries, and administrative records, creating a detailed dataset for thorough analysis. Subsequently, algorithms are employed to detect patterns and trends within this data, such as examining patient demographics and medical histories to identify potential health risks. The final step involves predicting outcomes based on the analyzed data, such as flagging patients at higher risk for chronic conditions or determining which treatments are likely to be most effective.
This meticulous process ensures that the predictions are based on comprehensive and accurate information, enhancing the reliability of the insights provided. By leveraging advanced algorithms and statistical models, healthcare providers can focus on data-driven strategies to improve patient outcomes. This systematic approach to analyzing and predicting health trends underscores the importance of data integrity and the need for consistent data collection and maintenance. The predictive analytics process ultimately fosters a proactive approach in healthcare, enabling earlier interventions and personalized treatment plans tailored to individual patient needs.
Applications of Predictive Analytics in Healthcare
Personalized Care and Treatment Plans
Applications of predictive analytics span various facets of healthcare, from personalized care to managing public health. In supporting personalized care, predictive analytics equips doctors with the insights necessary to design treatment plans tailored to individual patient needs. These insights, drawn from medical histories, genetic data, and other factors, lead to more accurate diagnoses and effective treatment decisions. For example, predictive analytics can help identify the most appropriate cancer treatment based on a patient’s genetic profile, improving treatment outcomes and minimizing the side effects.
Personalized care extends beyond treatment plans to include preventive measures. By predicting which patients are at risk for specific conditions, healthcare providers can implement early interventions, thereby preventing or mitigating the severity of diseases. Individuals with a high genetic predisposition to certain conditions can be monitored more closely, ensuring that they receive timely and targeted preventive care. This approach helps in reducing overall healthcare costs by preventing expensive treatments and hospital stays, promoting a higher quality of life for patients, and delivering more effective healthcare services.
Monitoring Population Health
Monitoring population health is another critical application, where predictive models provide early warnings about disease outbreaks, enabling prompt and well-prepared responses. The case of BlueDot’s early detection of COVID-19 exemplifies the significant role predictive analytics can play in safeguarding public health. By rapidly analyzing global data sources, predictive models can identify emerging health threats before they escalate into widespread epidemics, allowing public health authorities to take preemptive measures.
This capability is particularly valuable in managing pandemics and other large-scale health crises. Predictive analytics can inform resource allocation, guiding where to deploy medical supplies and personnel most effectively. Additionally, these models can help track the effectiveness of interventions, providing real-time data on infection rates and response efficacy. This ensures that health organizations remain agile and prepared to address new challenges, ultimately improving the resilience of public health systems and saving lives through timely action.
Managing Chronic Diseases
Predictive analytics is instrumental in reducing the burden of chronic diseases like diabetes and heart disease. By analyzing factors such as lifestyle, medical history, and coexisting health issues, predictive models identify individuals at risk, enabling early intervention. This preemptive approach leads to better health outcomes and cost reduction over time. For instance, predictive models can alert healthcare providers to patients who are likely to develop complications, allowing for proactive management of their conditions and avoiding costly emergency treatments.
The ability to predict and manage chronic diseases plays a crucial role in enhancing patient quality of life. Individuals at risk receive targeted advice and support for lifestyle changes, medication management, and regular monitoring, reducing the likelihood of severe health episodes. This continuous care model, supported by predictive analytics, fosters a collaborative relationship between patients and healthcare providers, empowering patients to take an active role in their health. As a result, chronic disease management becomes more efficient and effective, benefiting both patients and healthcare systems.
Operational Efficiency and Cybersecurity
Enhancing Hospital Operations
Hospitals, constantly grappling with challenges like staffing shortages and equipment downtime, also benefit from predictive analytics. It enables them to forecast patient admissions accurately, optimize staff scheduling, and predict maintenance needs for medical equipment, thereby improving operational efficiency and care delivery. By anticipating patient volumes, hospitals can ensure they have adequate resources and personnel to handle demand, reducing wait times and enhancing patient satisfaction.
Optimizing operations also involves streamlining administrative processes. Predictive analytics can identify bottlenecks in patient flow, uncover inefficiencies in resource utilization, and suggest improvements. This data-driven approach helps hospitals allocate their resources more effectively, mitigating issues such as overcrowded emergency rooms or prolonged hospital stays. Enhanced operational efficiency ultimately translates to better patient care and more sustainable healthcare systems, highlighting the importance of integrating predictive analytics into hospital management.
Strengthening Cybersecurity
Enhancing cybersecurity is another crucial application of predictive analytics in healthcare, an industry increasingly targeted by cyberattacks. Predictive models identify potential vulnerabilities, monitor system activities, and assign risk levels to various transactions, reducing the likelihood of breaches and protecting sensitive patient information. With the growing digitization of healthcare data, robust cybersecurity measures are essential to ensure data integrity and maintain patient trust.
The use of predictive analytics in cybersecurity goes beyond threat detection to include proactive risk management. By continuously analyzing network traffic and user behavior patterns, predictive models can forecast potential threats and implement preventative measures. This approach helps healthcare organizations stay ahead of cybercriminals, safeguarding their IT infrastructure and confidential patient data. Ensuring robust cybersecurity through predictive analytics is vital for maintaining the reputation of healthcare providers and ensuring uninterrupted service delivery.
Real-World Success Stories
Reducing Readmissions and Costs
Successful implementations of predictive analytics across different healthcare settings highlight its impact. For instance, Corewell Health utilized predictive models to identify patients at high risk of readmission, subsequently providing customized follow-up care, saving $5 million, and significantly reducing readmissions. This example underscores how predictive analytics can enhance patient outcomes while simultaneously reducing healthcare costs, emphasizing the potential for widespread benefits.
Other healthcare organizations have similarly leveraged predictive models to achieve notable results. By focusing on high-risk patient cohorts, they can implement targeted interventions that prevent complications and improve overall health outcomes. This proactive approach leads to cost savings and more efficient resource utilization. Healthcare providers can reallocate conserved resources to other areas of need, further improving patient care and operational sustainability. These success stories demonstrate the tangible benefits of integrating predictive analytics into healthcare practices.
Early Disease Detection
Machine learning models are now capable of predicting conditions such as Alzheimer’s disease and diabetes years before symptoms appear. Additionally, predictive analytics has helped reduce appointment no-show rates in a pediatric hospital in Chile by over 10 percent through targeted reminders. Such applications reveal the transformative potential of predictive analytics in early disease detection and patient adherence, paving the way for more proactive and effective healthcare management.
Early disease detection significantly improves patient outcomes by allowing timely treatment and intervention. By identifying individuals at risk long before symptoms manifest, healthcare providers can implement strategies that delay or prevent the onset of disease altogether. This paradigm shift from reactive to proactive healthcare reduces the burden on healthcare systems and enhances patient quality of life. The success of predictive analytics in early detection underscores its critical role in modern medicine, offering hope for managing and potentially eradicating chronic and incurable conditions.
Challenges and Considerations
Clinician Acceptance and Usability
Despite its promise, the implementation of predictive healthcare analytics faces several significant challenges. Clinician acceptance remains a primary hurdle, as integrating predictive tools often imposes additional responsibilities, such as updating EHRs and interpreting data dashboards. Overcoming this resistance requires involving clinicians in the tool development process and incorporating their feedback to enhance usability and adoption. Training and support are essential to ensure that healthcare professionals can effectively leverage predictive analytics in their practice.
By demonstrating the tangible benefits of predictive analytics, healthcare organizations can foster a culture of acceptance and enthusiasm among clinicians. Highlighting successful case studies and providing continuous education on the evolving landscape of predictive technologies can further enhance buy-in. Addressing concerns about workload and usability through collaborative and iterative design processes creates tools that are more intuitive and integrated into existing workflows. This approach helps bridge the gap between technological advancements and practical application, maximizing the impact of predictive analytics on patient care.
Ethical Concerns and Algorithmic Bias
Addressing ethical concerns and algorithmic bias is paramount, as algorithms can reflect biases present in the training data, leading to inequities in care. Ensuring transparency, fairness, and conducting regular audits are crucial steps in mitigating these risks. By actively monitoring for bias and involving diverse stakeholders in the development process, healthcare organizations can promote equitable health outcomes, ensuring that predictive models benefit all patients.
Moreover, ethical considerations extend to data privacy and informed consent. Patients must be aware of how their data is being used and the implications of predictive analytics on their care. Establishing clear guidelines and maintaining open lines of communication with patients fosters trust and compliance. Ethical practices in the deployment of predictive analytics ensure that technology enhances, rather than undermines, patient care and public trust in healthcare systems. Regularly revisiting and updating ethical standards in light of new developments is necessary for maintaining high standards of patient care.
Regulatory and Legal Challenges
Regulatory and legal challenges also pose considerable obstacles. The absence of clear regulations for AI in healthcare introduces risks associated with inconsistent model performance and safety issues. Establishing internal policies to monitor and validate predictive models is essential to ensure reliable outcomes. Keeping abreast of evolving regulations and participating in policy development processes can help healthcare providers navigate these challenges effectively.
Proactively addressing legal concerns can mitigate potential liabilities and ensure compliance with industry standards. Developing comprehensive documentation and robust validation protocols for predictive models builds a foundation of accountability and transparency. Collaboration with regulatory bodies, policymakers, and industry leaders can further refine standards and practices, ensuring that predictive analytics is integrated smoothly and safely into healthcare environments. Anticipating and adapting to regulatory shifts strengthens the overall resilience and efficacy of predictive healthcare systems.
Data Privacy and Security
Data privacy and security are also critical, with healthcare data breaches becoming increasingly common; therefore, robust measures like encryption, monitoring, and adherence to regulations such as HIPAA are necessary to protect patient data and maintain trust. Healthcare organizations must prioritize cybersecurity, implementing state-of-the-art measures to safeguard sensitive information and ensure compliance with legal standards.
Investing in advanced security technologies and continuous monitoring systems can detect and respond to potential threats in real time. Training staff on best practices for data security and handling ensures that all members of an organization contribute to maintaining robust defenses. Adopting a comprehensive and proactive approach to data privacy not only protects patient information but also enhances the reputation and reliability of healthcare providers. These efforts are crucial for fostering a trustworthy environment where predictive analytics can thrive and deliver its full potential benefits.
Future Directions and Innovations
Advances in AI
The analysis of patient care has greatly advanced with the abundance of data available today. Predictive healthcare analytics leverages various data sources such as Electronic Health Records (EHRs), insurance claims, medical imaging, and health surveys. By tapping into these streams, predictive tools can, for instance, examine patterns in patient records to predict the likelihood of hospital readmissions or evaluate medication adherence to foresee the onset of chronic diseases. This leads to more effective and timely interventions by healthcare providers. Furthermore, predictive analytics helps healthcare professionals navigate patient records more efficiently, enabling targeted interventions and streamlining healthcare processes.
Merging different data sources can give a comprehensive view of a patient’s health journey. Integrated data from EHRs and medical imaging can reveal patterns that might be missed when looking at a single data source. Predicting diseases like heart conditions or diabetes becomes possible by analyzing diverse datasets together, offering a holistic view. This empowers healthcare providers to make well-informed decisions, optimizing patient care and reducing risks linked to delayed diagnosis and treatment.