In recent years, an innovative approach to type 1 diabetes treatment has gained significant attention, bringing newfound hope to millions. Spearheaded by international scientists, this development involves the use of 3D printed human islets, offering a groundbreaking alternative to traditional methods. These meticulously manufactured islets promise a future where routine insulin injections could become a relic of the past. This shift not only marks a remarkable scientific triumph but also is shaping up as a potential game-changer in the way diabetes is managed, aiming to enhance patient comfort and treatment efficacy.
The Science Behind 3D Printed Islets
Creating a Functional Structure
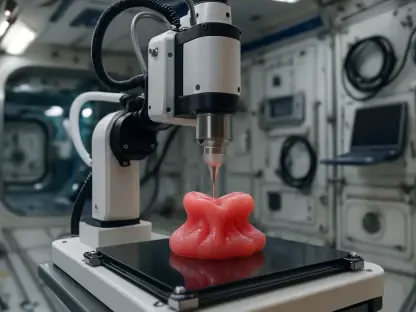
The innovative technique of 3D printing human islets hinges on crafting a functional structure that closely mimics the natural pancreatic environment, crucial for the islets’ survival and functionality. Each islet is printed using a specialized bio-ink made of alginate combined with decellularized human pancreatic tissue. This combination fosters a dense yet porous structure, promoting optimal oxygen and nutrient flow to the cells within. The intricate design facilitates better vascularization, which is essential for maintaining cell health post-transplantation. While conventional techniques struggle with inconsistent cell survival, this advancement addresses those issues through its emphasis on biomimicry.
The team, led by Dr. Quentin Perrier, focused on ensuring the islets’ design closely resembled native pancreatic architecture. Their aim was to enhance the survival and insulin-releasing efficiency of the cells upon transplantation. During laboratory tests, these printed islets showcased an impressive glucose response, adjusting insulin secretion levels accordingly. With experiments yielding a cell survival rate of 90%, the robustness of this approach shines through, emphasizing its potential over current alternatives. The meticulously controlled environment provided by the bio-ink significantly mitigates challenges posed by traditional transplantation methodologies.
Testing and Response in Laboratory Conditions
In laboratory settings, the performance of these 3D printed islets has been nothing short of promising. They successfully demonstrated an ability to detect and respond to varying glucose concentrations, releasing insulin amounts suitable for the body’s needs. This indicates a level of functionality comparable to natural islets, addressing major limits of existing therapies. The controlled lab conditions mirrored potential in vivo scenarios, offering insights into how these cells might behave post-implantation. Such demonstrations provide a strong foundation for understanding the practical applicability of this breakthrough.
The innovative response mechanisms of these islets suggest a significant leap forward in diabetes treatment. Traditional transplants often face various obstacles, including high cell loss and reliance on donor availability. The manufactured islets not only overcome donor dependency but also circumvent the complexities tied to conventional procedures. As the research progresses, questions regarding their long-term efficacy compared to natural islets remain at the forefront of scientific inquiry. However, the initial results have set a foundation for growing optimism, paving a likely path to drastically reduced dependency on daily insulin injections.
Comparative Advantages Over Traditional Methods
Reduced Complexity and Invasiveness
Traditional islet transplantation is fraught with complexities and barriers, notably its reliance on a small pool of compatible donors and the considerable risks associated with the procedure. The painstaking extraction and transplantation of islets involve high costs and often result in significant cell loss. In contrast, 3D printed islets present a streamlined alternative, offering a safer and less invasive procedure. By allowing islets to be implanted subcutaneously under local anesthesia, patients experience reduced discomfort and lower risks of complications, enhancing the overall treatment experience.
The shift to a less invasive approach marks a pivotal departure from conventional procedures. As 3D printed transplantations predominantly occur beneath the skin, the need for extensive surgical intervention nearly vanishes. This reduces hospitalization times and the associated logistical challenges for patients and healthcare providers. Furthermore, with less reliance on anesthesia and other complexities, patients can enjoy a quicker recovery, effectively improving their overall quality of life and ensuring adherence to the treatment plan. Such benefits emphasize the practicality and value of this technological progression.
Implications for Future Treatment
While these developments hold great promise, the full potential of 3D printed islets in replacing daily insulin injections remains to be seen. The scope of their application is vast, suggesting a possible future where diabetes treatment becomes simpler and more accessible. Ongoing research aims to refine these methods, potentially leading to “off-the-shelf” treatments readily available to patients worldwide. This could mark a paradigm shift in how diabetes is managed, offering significant life improvements by reducing or eliminating the daily burden of insulin administration.
Dr. Perrier emphasizes the importance of using human insulin cells in these advances, rather than animal derivatives typically seen in conventional approaches. This choice not only enhances compatibility but also highlights the broader implications for future clinical applications. Such innovations are set to redefine diabetes care standards, ensuring more effective and personalized treatment options for patients. As the exploration continues, it carries with it the potential to transform the landscape of chronic disease management, underscoring the remarkable evolution of biotechnology and its real-world implications.
A New Dawn for Diabetes Management
In recent years, an exciting breakthrough in the treatment of type 1 diabetes has emerged, capturing the attention of millions and instilling new hope. Led by a collaborative team of international scientists, this groundbreaking advancement employs the revolutionary technology of 3D printing to create human islets, providing an innovative alternative to the traditional treatment options available. These meticulously crafted islets present the possibility of a future where the daily routine of insulin injections might become a thing of the past, revolutionizing diabetes management. This development signifies not just a major scientific achievement but also promises to transform how diabetes is managed, enhancing patient comfort and boosting the effectiveness of treatment. The approach could redefine the patient experience and lead to improved outcomes by focusing on personalized and precise management strategies, opening doors to an era where diabetes care is both advanced and accessible for individuals worldwide.