In the rapidly advancing realm of medical innovation, cell and gene therapies stand out as potential game-changers for treating life-threatening diseases, yet they face formidable obstacles on the path to market. The U.S. Food and Drug Administration (FDA) has increasingly postponed or denied approvals due to persistent issues in chemistry, manufacturing, and controls (CMC), a cornerstone of ensuring product safety and reliability. These regulatory roadblocks not only slow down the delivery of cutting-edge treatments to patients but also expose a critical disconnect between the pace of scientific discovery and the practical demands of scalable production. As developers race to address unmet medical needs, the mounting delays signal a pressing need for stronger manufacturing frameworks to match the ambition of these therapies. This tension between innovation and execution continues to shape the landscape, raising questions about how the industry can adapt to meet stringent standards while maintaining momentum in development.
Regulatory Challenges in Cell and Gene Therapy Approvals
CMC as a Leading Cause of FDA Delays
The prevalence of CMC deficiencies has emerged as a dominant factor in the FDA’s decisions to delay or reject cell and gene therapy applications, casting a shadow over the field’s progress. Data indicates that a striking 74% of Complete Response Letters (CRLs)—formal notices from the FDA signaling that an application cannot be approved as submitted—issued in recent years pointed to manufacturing and quality control shortcomings. These letters often require developers to provide additional data or rectify specific issues before resubmission. The impact is evident in cases like Ultragenyx’s gene therapy for Sanfilippo syndrome type A, where manufacturing gaps halted approval despite promising clinical insights. Similarly, Capricor’s cell therapy for Duchenne muscular dystrophy faced rejection due to insufficient CMC documentation alongside clinical data concerns. These examples underscore how even therapies with significant potential can stumble when production processes fail to meet regulatory benchmarks, prolonging the wait for patients in desperate need.
Beyond individual cases, the broader trend of CMC-related rejections reveals systemic challenges within the industry that hinder timely approvals. The FDA’s rigorous scrutiny of manufacturing processes aims to safeguard patient safety and ensure consistent therapeutic outcomes, but it often catches developers off guard. Many companies, particularly smaller or less experienced ones, struggle to anticipate the depth of detail required in CMC submissions, leading to costly delays. For instance, inconsistencies in batch production or inadequate validation of manufacturing steps can trigger CRLs, forcing firms to overhaul processes at significant expense. This pattern not only slows down specific therapies but also sends a clear message to the sector: robust manufacturing must be prioritized alongside clinical development to avoid regulatory setbacks. As the number of applications for advanced therapies grows, addressing these CMC hurdles becomes paramount to maintaining trust in the regulatory process and delivering treatments efficiently.
Impact of Accelerated Approval Pathways
Accelerated approval pathways, designed to expedite access to therapies for serious conditions with unmet needs, introduce a complex dynamic to the CMC challenge faced by developers. These programs, often relying on surrogate endpoints rather than long-term clinical outcomes, aim to shorten the timeline from lab to patient by compressing clinical phases. However, this speed comes at a cost, as the reduced window leaves little room to refine manufacturing processes adequately. Industry voices, such as Dr. Clare Blue from eXmoor Pharma, describe this as a precarious balance, where the urgency to address critical health issues can undermine the readiness of CMC frameworks. The result is a heightened risk of regulatory rejection, as the FDA maintains strict standards regardless of the accelerated timeline, pushing developers to juggle rapid clinical progress with the intricate demands of production quality.
Moreover, the pressure of accelerated pathways often amplifies existing gaps in manufacturing expertise and resources, further complicating the path to approval. Developers may focus heavily on meeting clinical milestones to secure investor support or demonstrate therapeutic potential, inadvertently sidelining the detailed work needed for CMC compliance. When CRLs are issued due to manufacturing flaws under these tight schedules, the setback can be particularly devastating, as timelines are already condensed. The FDA’s insistence on comprehensive data integrity and process validation does not waver, even under fast-track conditions, meaning that companies must find ways to align their manufacturing strategies with clinical urgency. This scenario highlights the necessity of integrating robust production planning from the earliest stages, even when the allure of accelerated approval tempts a focus on speed over substance, to prevent costly regulatory delays.
Manufacturing Complexities and Early-Stage Decisions
Critical Role of Initial Development Choices
The foundation of successful cell and gene therapy development often lies in the seemingly mundane decisions made during the earliest phases, which can profoundly influence later regulatory outcomes. Choices such as cell sourcing, vector selection, and initial process design set the trajectory for manufacturability and scalability, yet they are frequently made with limited foresight into commercial demands. Unlike traditional small-molecule drugs, where manufacturing tweaks can be implemented with relative ease, advanced therapies face significant hurdles when adjustments are needed, often at prohibitive costs. Dr. Bo Wiinberg from the Novo Nordisk Foundation Cellerator stresses that scalability must be embedded in the design from the outset, as retrofitting processes to meet larger production needs can lead to delays or even derail projects entirely. These early missteps can compound over time, creating bottlenecks that the FDA flags during review.
Equally important is the recognition that early-stage decisions are not just technical but strategic, shaping the entire lifecycle of a therapy’s journey to market. For instance, opting for a specific cell line or production method without considering long-term supply chain stability can result in inconsistencies that regulators scrutinize heavily. The complexity of these therapies means that each component must be meticulously validated, a process that becomes exponentially harder if foundational choices are flawed. Developers who fail to anticipate the rigors of late-stage manufacturing often find themselves forced into expensive redesigns or unable to meet FDA expectations for consistency and quality. This underscores the need for a forward-thinking approach, where collaboration with manufacturing experts during initial planning can prevent the pitfalls of short-sighted decisions, ensuring a smoother path through the regulatory maze and ultimately benefiting patient access.
Lack of Standardization and Expertise
One of the most persistent barriers in scaling cell and gene therapies lies in the absence of standardized manufacturing processes, a challenge exacerbated by the bespoke nature of each product. Unlike conventional pharmaceuticals, where established protocols can streamline production, advanced therapies often demand unique approaches tailored to specific biological mechanisms. This individuality complicates efforts to create uniform guidelines, leaving developers to navigate uncharted territory with each new therapy. Additionally, the limited pool of contract development and manufacturing organizations (CDMOs) with proven expertise in this niche field adds to the strain. Many firms lack access to partners capable of handling the intricacies of late-stage production, resulting in CMC submissions that fall short of regulatory expectations and contribute to approval delays.
Compounding this issue is the risky tendency among some developers to submit incomplete CMC data, banking on the possibility of addressing deficiencies after initial approval—a strategy that rarely succeeds under current FDA oversight. The agency’s heightened focus on upfront validation means that gaps in manufacturing documentation are often grounds for rejection, as seen in numerous CRLs. Without standardized platforms or widely available expertise, companies frequently struggle to anticipate the full scope of regulatory requirements, leading to costly rework. This situation highlights a critical industry gap: the need for more accessible resources and shared knowledge to support consistent manufacturing practices. Until such frameworks emerge, developers must rely on meticulous internal planning and seek out specialized CDMOs, despite the scarcity, to build the robust processes necessary for navigating the stringent approval landscape.
Evolving FDA Expectations and Industry Responses
Rising Regulatory Standards
As the field of cell and gene therapies expands, the FDA has responded with increasingly stringent standards for manufacturing quality, reflecting a commitment to patient safety and therapeutic reliability. This trend of heightened scrutiny focuses on data integrity, process validation, and consistency across production batches—elements that are non-negotiable in the agency’s evaluation process. The shift signals a clear message to developers: clinical innovation alone is insufficient without a parallel emphasis on manufacturing excellence. Experts across the sector agree that aligning CMC strategies with late-stage and commercial objectives from the beginning is no longer optional but essential. This proactive stance is critical to meeting the FDA’s evolving benchmarks, which aim to ensure that therapies not only show promise in trials but can be reliably produced at scale for widespread use.
Furthermore, the tightening of regulatory expectations has reshaped how companies approach the development lifecycle, pushing for earlier investment in manufacturing infrastructure. The days of treating CMC as an afterthought are fading, as the FDA’s focus on detailed documentation and robust validation processes becomes more pronounced. Developers now face the challenge of balancing resource allocation between clinical research and production readiness, often under constrained budgets. The consensus is that engaging with regulators throughout the development journey—leveraging past feedback and maintaining open dialogue—can help align efforts with agency priorities. This shift toward stricter standards, while daunting, serves as a catalyst for the industry to elevate its practices, ensuring that only therapies meeting the highest quality thresholds reach patients, thereby fostering greater confidence in these transformative treatments.
Technological Innovations as Potential Solutions
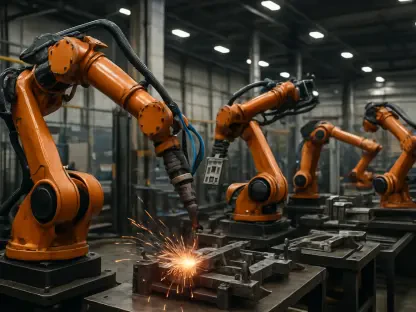
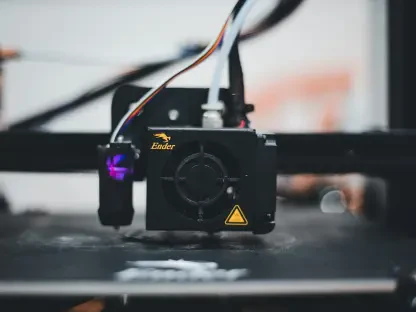
Amid the challenges posed by CMC issues, technological advancements offer a glimmer of hope for streamlining manufacturing and meeting the FDA’s rigorous demands. Tools such as artificial intelligence (AI), automation, and Process Analytical Technology (PAT) are gaining traction as means to enhance process understanding and reduce variability in production. AI, for instance, can analyze vast datasets to predict potential manufacturing hiccups before they occur, while automation minimizes human error in complex processes. PAT enables real-time monitoring of critical quality attributes, ensuring consistency across batches. These innovations hold the potential to bridge gaps in current capabilities, providing developers with the precision needed to satisfy regulatory requirements and accelerate the path to approval without compromising on safety or efficacy.
Looking ahead, the adoption of these cutting-edge tools could pave the way for greater standardization in a field historically defined by bespoke solutions, reshaping how therapies are brought to market. While full implementation remains in progress, early adopters report improved control over manufacturing variables, a key factor in addressing FDA concerns. However, integrating such technologies requires significant investment and expertise, posing a barrier for smaller developers. Nevertheless, the promise of reducing CMC-related delays through enhanced process validation is driving interest across the industry. As these tools mature, they may offer a scalable framework for production, easing the burden of meeting rising regulatory standards. The focus now lies in fostering collaboration between tech innovators and therapy developers to ensure these solutions are accessible, ultimately smoothing the regulatory journey for groundbreaking treatments awaiting patient access.