I’m thrilled to sit down with Kwame Zaire, a renowned manufacturing expert whose deep knowledge of electronics, equipment, and production management has made him a thought leader in the pharmaceutical industry. With a particular focus on predictive maintenance, quality, and safety, Kwame brings a unique perspective to the rapidly evolving world of cell and gene therapy. Today, we’ll dive into the challenges and innovations shaping this dynamic field, exploring topics like navigating rapid advancements, scaling manufacturing, balancing speed with safety, and adapting to industry headwinds and emerging technologies.
How do you see the cell and gene therapy landscape evolving, and what are the most significant shifts you’ve noticed in recent years?
The cell and gene therapy space is transforming at an incredible pace. We’re seeing groundbreaking therapies move from concept to clinical reality faster than ever, which is both exciting and challenging. One of the biggest shifts is the sheer speed of innovation—new modalities like nucleic acids and lipid nanoparticles are emerging alongside established viral vectors. Another key change is the focus on patient access, especially with therapies like CAR-T, where manufacturing bottlenecks are limiting treatment to just a fraction of eligible patients. It’s a field that’s pushing boundaries, but it’s also forcing us to rethink how we design and scale production processes to keep up.
There’s a saying in the industry about ‘building the plane as we’re flying it.’ Can you unpack what that means for day-to-day operations in this fast-paced environment?
Absolutely. That phrase captures the essence of working in advanced therapies—everything is moving so quickly that we’re often developing processes and solutions while implementing them. In daily operations, it means constantly adapting to new data, client needs, or regulatory updates. For instance, we might be setting up a manufacturing line for a therapy while still refining the process based on trial results. It’s a dynamic, sometimes chaotic approach, but it’s necessary to keep therapies moving toward patients who need them urgently.
What are some of the toughest challenges that come with this rapid innovation in cell and gene therapy?
One of the toughest challenges is the uncertainty that comes with uncharted territory. We’re dealing with therapies that are highly personalized and complex, so small changes in a process can have big downstream effects. There’s also the pressure to move fast—clients want therapies to market quickly—but we can’t compromise on quality or safety. Another hurdle is the talent and expertise needed; these therapies require specialized skills that aren’t always easy to find or scale. It’s a constant balancing act to innovate without overextending resources or risking patient outcomes.
Speaking of balance, how do you ensure safety and quality standards are met when speed is such a critical factor?
Safety and quality are non-negotiable, no matter the timeline. We achieve this by embedding rigorous checks into every stage of development and production. Predictive maintenance, for example, plays a huge role—by using data to anticipate equipment issues before they happen, we prevent disruptions that could compromise a batch. We also rely on standardized protocols where possible, even if the therapy itself is novel, to create a foundation of reliability. And honestly, it’s about fostering a culture where every team member knows that cutting corners isn’t an option, no matter the deadline.
The industry has faced some setbacks, like contract losses or slower program ramps. How do you approach stabilizing a business amidst these kinds of headwinds?
Setbacks are part of any evolving industry, especially one as complex as this. Stabilization starts with focusing on the core strengths—ensuring that outside of specific issues, the broader business operations are robust. That means diversifying client portfolios to avoid over-reliance on a single contract and investing in process improvements that build efficiency. Communication with clients is also key; being transparent about challenges and proactive with solutions helps maintain trust. Ultimately, it’s about resilience—using setbacks as a chance to refine strategy rather than just reacting to them.
Pipeline rationalization is a hot topic as biopharma companies narrow their focus. How do you adapt to support clients who are prioritizing certain programs over others?
Pipeline rationalization is definitely reshaping how we work with clients. Our role is to be a flexible partner, aligning our resources and expertise with the programs they deem most promising. We focus on adding value by offering tailored solutions—whether that’s optimizing manufacturing for a specific therapy or providing data-driven insights to de-risk their decisions. It’s also about staying agile; we need to anticipate shifts in their priorities and be ready to pivot quickly, whether that means scaling up support for a key asset or winding down efforts on a deprioritized one.
Scaling manufacturing capacity seems to be a persistent hurdle in this space. Why is it so difficult to scale up production for therapies like CAR-T?
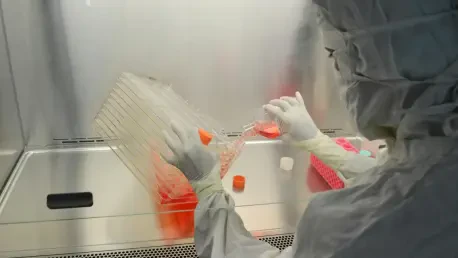
Scaling in cell and gene therapy is tough because these therapies are often highly individualized—think of CAR-T, where cells are taken from a patient, modified, and returned. That process doesn’t lend itself to traditional mass production. Every batch is essentially a custom job, requiring strict control over variables like cell viability and contamination risk. Plus, the infrastructure for large-scale production—specialized facilities, trained staff, and supply chains for raw materials—takes significant time and investment to build. Until those pieces are in place, scaling remains a bottleneck that directly impacts how many patients can access these life-changing treatments.
There’s been discussion about a hybrid approach to manufacturing capacity. What’s your perspective on balancing internal and outsourced production?
I think a hybrid approach makes a lot of sense in this industry. Building internal capacity gives companies control over critical aspects of their supply chain and ensures consistency for high-demand therapies. But maintaining that capacity full-time can be costly, especially if demand fluctuates. Outsourcing, on the other hand, offers flexibility—ramping up or down based on need without the overhead of idle facilities. The trick is finding the right balance: keeping core competencies in-house while leveraging trusted partners for overflow or specialized tasks. It’s a strategy that can help meet patient demand more effectively without overcommitting resources.
Innovative platforms are being developed to accelerate development in areas like viral vector manufacturing. How do these tools change the game for speeding up timelines?
These platforms are game-changers because they streamline complex processes that used to take months or even years. For viral vector manufacturing, for instance, standardized platforms can cut down on development time by providing pre-validated frameworks—think of them as a blueprint that reduces trial and error. They also lower costs by minimizing the need for bespoke solutions for every project and reduce risks by ensuring consistency across batches. Ultimately, they allow us to get therapies to clinical stages faster, which is critical for patients waiting on these treatments.
Looking ahead, what is your forecast for the future of cell and gene therapy manufacturing over the next decade?
I’m optimistic about the next decade, though it won’t be without challenges. I expect we’ll see significant advancements in automation and digital tools that make manufacturing more efficient and scalable—think AI-driven process optimization or real-time monitoring systems. We’ll also likely see more therapies approved, which will put even greater pressure on solving scaling issues. The industry will need to collaborate more—between CDMOs, biopharma, and regulators—to standardize where possible without stifling innovation. My forecast is that by 2030, we’ll have cracked some of these persistent bottlenecks, making therapies more accessible, but it’ll take a collective push to get there.