Kwame Zaire stands at the forefront of manufacturing innovation, particularly in the realm of electronics and equipment. His expertise spans production management to the critical aspects of predictive maintenance, quality, and safety. Today, we delve into the world of metal Additive Manufacturing (AM) for medical applications, focusing on custom orthopaedic implants. Kwame sheds light on how HBD is transforming this industry with cutting-edge technology.
Can you explain how HBD’s Laser Beam Powder Bed Fusion (PBF-LB) technology works and its benefits for manufacturing orthopaedic implants?
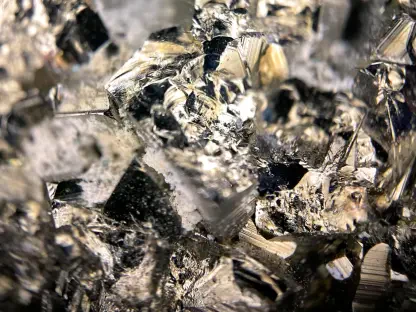
HBD’s Laser Beam Powder Bed Fusion (PBF-LB) is a sophisticated process that focuses on layering powdered metal and fusing it using a laser beam. This technique allows for precise control over the material, resulting in high-quality and intricate designs that are often necessary for orthopaedic implants. The benefits are substantial; producing implants with complex geometries and customized features becomes possible, which significantly enhances fit and function in medical applications.
What are the specific challenges in traditional orthopaedic implant manufacturing that HBD’s technology aims to address?
Traditional orthopaedic manufacturing faces several setbacks, notably high material wastage and prolonged delivery cycles. Conventional machining tends to utilize only 30-40% of material, leading to significant wastage. Delivery cycles can be lengthy, spanning 6-8 weeks due to numerous stages like milling and post-processing. Inconsistent product quality is another challenge, largely due to manual polishing and welding processes that introduce defects. HBD’s AM technology addresses these issues by streamlining the process to achieve higher material utilization and faster production cycles with consistent quality.
How does the use of medical-grade TC4 titanium alloy enhance the biocompatibility of the implants?
The use of medical-grade TC4 titanium alloy is crucial for ensuring biocompatibility in implants. This material is known for its non-toxic and non-immunogenic properties, making it ideal for integration within the human body. It supports cellular growth and functions without adverse reactions, which is indispensable in orthopedic applications where implant acceptance and integration with the body are paramount.
Could you describe the significance of the bionic porous lattice structures in the implants?
Bionic porous lattice structures are a revolutionary feature in implant design. These structures mimic natural bone porosity, allowing for better mechanical stability and biological integration. Pore sizes ranging from 0.5-1 mm provide optimal conditions for bone growth and integration, making the implants more functional and supportive of natural healing processes. The interconnected pores facilitate nutrition and oxygen flow which improves the regenerative processes of the bone.
How do the production times for the talar and radial implants on HBD machines compare to traditional methods?
Production times for talar and radial implants undergo significant reduction using HBD machines. The talar implant takes about five hours on the HBD 150 machine at a precision layer thickness of 30 μm, while the radial prosthesis is completed in nine hours on the HBD 200 machine. Traditional methods cannot match these times, often requiring several weeks due to multi-stage processes.
In what ways did HBD collaborate with South China University of Technology and Guangzhou First People’s Hospital for complex reconstructive surgeries?
HBD’s collaboration involved using AM technology to develop patient-specific solutions for complex cases, such as the developmental hip dysplasia. By partnering with South China University of Technology and Guangzhou First People’s Hospital, HBD utilized CT imaging alongside patient anatomical data to create tailored implants. This collaboration exemplifies how cutting-edge technology can solve real-world challenges in surgical reconstruction by ensuring precision and personalized fitment.
Could you elaborate on the creation of the titanium hip spacer for the developmental hip dysplasia case?
The creation of the titanium hip spacer involved several steps, starting with CT imaging to capture detailed anatomical data. This data was used to design a custom-fit porous structure aimed at aligning with the patient’s bone geometry. The tailored approach aided in precise fitting, promoted bone regeneration, and provided post-operative symmetry and stability. This case highlighted the importance of integrating technology and patient-specific data for successful surgical outcomes.
How does HBD ensure precision and quality at scale, especially in larger batch productions with machines like the HBD 350 and HBD 400?
HBD’s larger machines, the HBD 350 and HBD 400, are engineered to maintain precision and quality even at scale. They incorporate advanced controls and monitoring systems to ensure that each layer and structure is produced to the exact specifications required. By embracing automation and real-time quality checks, HBD guarantees consistency and excellence in batch production.
In what other medical areas or scenarios can HBD’s technology be applied, beyond orthopaedic implants?
HBD’s AM technology holds potential beyond orthopaedic implants; it can be effectively used in dental implants and customizable surgical tools. The precision and adaptability offered by this technology open new avenues for personalized medical solutions, such as cranial or facial implants and prosthetics that require complex geometries and biocompatible materials.
What future advancements or innovations is HBD working on to further improve orthopaedic implant manufacturing?
HBD is continuously advancing its efforts to enhance orthopaedic implant manufacturing. Future innovations may include refining the material properties for better performance, integrating AI for predictive modeling in the design phase, and expanding the capabilities of their machines to produce even more complex and personalized implants rapidly. These efforts aim to push the boundaries of AM technology, optimizing outcomes for patients and medical practitioners alike.